
What is a retinal detachment?
A retinal detachment occurs when the neurosensory retina is separated from the retinal pigment epithelium. When the retina detaches, the process is similar to when wallpaper peels away from the living room wall. If you develop a retinal detachment, you will almost certainly need to undergo an operation to reattach the retina.
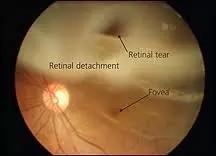
Most cases of retinal detachments are rhegmatogenous in nature. This means that the retina detached because of a retinal tear (or more). This tear allows fluid to track under the neurosensory retina, thus separating the neurosensory retina from the retinal pigment epithelium.
The aim of retinal detachment surgery is to ‘glue’ the neurosensory retina back where to it is meant to be positioned. During the operation, the fluid between the neurosensory retina and retinal pigment epithelium will be drained out, so that both layers can be pushed back together.
Surgery can be complicated and may take around 1 to 2 hours. Although retinal detachment surgery can be performed safely with local anesthesia, some people prefer to have surgery under general anesthesia. You should choose the anesthetic option that you are most comfortable with. These days, day case surgery is the norm and you should be able to go home the same day after surgery if you prefer.
Is retinal detachment surgery always necessary?
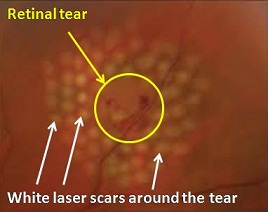
If you have a retinal tear, and this has not yet progressed to become a retinal detachment, you may be able to avoid having to undergo surgery provided the retinal tear is dealt with early enough. If the retinal tear is not too big and there isn’t too much hemorrhage obscuring its view, it can be successfully treated with laser retinopexy.
In laser retinopexy, laser ‘burns’ are applied all around the tear. This ‘fuses’ the neurosensory retina with the retinal pigment epithelium, and seals off the retinal tear. Fluid is prevented from accumulating under the neurosensory retina, thereby preventing the retina from detaching. For laser retinopexy to be successful, the laser burns must be applied as soon as possible around the tear before retinal detachment develops.
Types of retinal detachment surgery
It is not always possible to detect a retinal tear early enough before the retina detaches. When you are diagnosed with retinal detachment, you will be advised on one of the two main types of retinal detachment surgery procedures (which can be combined together if required): vitrectomy and scleral buckling surgery. Both techniques have a high success rate if performed appropriately and early enough.
Ideally, the retinal detachment should be repaired before the macula (central part of the retina) becomes detached and your central vision becomes affected. The later you postpone surgery, the lower the chances of success due to scarring from proliferative vitreoretinopathy. If your detached retina is not repaired, you will eventually lose all your vision in that eye.
Vitrectomy: This procedure is considered as the ‘internal approach’ for retinal detachment surgery because it involves the removal of the vitreous humor gel from inside the vitreous cavity of the eyeball. By removing the vitreous gel, there will no longer be areas of the retina that is being pulled by the vitreous. This is important to prevent the retina from developing other tears due to vitreous gel tugging on it.
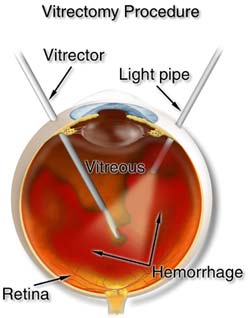
Vitrectomy surgery involves creating 3 entry sites (or ‘ports’) into the vitreous cavity. One port is for continuous infusion of balanced salt solution into the vitreous cavity. This to maintain the pressure within the eyeball and to prevent the eye from collapsing. The other 2 ports are for the insertion of instruments into the vitreous cavity, usually a light pipe and a vitreous cutter. The light pipe provides light for viewing. The vitreous cutter clears the vitreous gel and any associated blood. At the end of surgery, these 3 entry sites need to be stitched up tightly to prevent leakage.
After the vitreous is removed, fluid can be drained from under the neurosensory retina to ‘flatten’ it. Once the neurosensory retina is flattened and positioned back to where it should be, the vitreous cavity of the eyeball is filled with either gas or silicone oil. The gas and silicone oil are tamponade agents that keep the neurosensory retina pressed against the retinal pigment epithelium. Tamponade agents hold the retina in place by providing internal pressure to prevent the neurosensory retina from peeling off again.
If you have silicone oil in your eye, you will need to undergo another operation around 3 months later to remove the oil. If you have gas in the eye, you will avoid having another operation because the gas will absorb over 4 to 6 weeks. During this time, you should not fly because the decompressed air cabin will cause the gas in your eyeball to expand and increase your eye pressure tremendously. This can be excruciatingly painful. And also very bad for your optic nerve, particularly if you have glaucoma.
Scleral buckling: This procedure is considered as the ‘external approach’ for retinal detachment surgery because it uses a piece of plastic or silicone or sponge to press on the outside of the eye. This causes the sclera to ‘buckle’ inwards and forces the retinal pigment epithelium to press against the detached neurosensory retina.
This inward pressure forces fluid between the neurosensory retina and retinal pigment epithelium to exit through the pre-existing retinal tear. The inward pressure also relieves any vitreous gel traction on the retina. This stops the vitreous gel from further pulling on the retinal tear, thus preventing the tear from extending. Once placed, the piece of plastic or sponge is usually not removed and is not visible once surgery is finished.
Scleral buckling may be more suitable for less extensive retinal detachments in younger patients. This is because it causes less cataract when compared to vitrectomy surgery. However, scleral buckling is associated with its own problems, such as double vision and extrusion.
Cryopexy / Laser retinopexy: These are additional procedures that your ophthalmologist may perform when repairing your retinal detachment. The aim is to create a scar between the neurosensory retina and retinal pigment epithelium. The effectively ‘seals’ the retina and prevents fluid from seeping between the neurosensory retina and retinal pigment epithelium. This can be done with a freezing probe (cryopexy) or laser (laser retinopexy). The areas most commonly treated are around the retinal tear and also around the entire detached retina.
What can you expect after retinal detachment surgery?
After retinal detachment surgery, your eye will feel uncomfortable and your vision will be blurry for the next few days. In fact, this discomfort and blurriness can last for up to six weeks or more. During this time, you will be given antibiotic eye drops to reduce the risk of infection and steroid eye drops to settle down the inflammation in your eye.

Sometimes after retinal detachment surgery, you may be asked to posture. This involves sitting or lying with your head in a specific position for up to 10 days. The purpose of posturing is so that the silicone oil or gas bubble in the vitreous cavity is able to provide optimal pressure on the part of the retina that is being reattached.
After retinal detachment surgery, you can read and watch television as usual even though your vision is blurred. Using your eyes will not affect how the eye recovers. In general, you should be able to do the normal things that you enjoy doing as long as there is little risk of contamination of the eye, such as from swimming or being in dusty environments.
Over the long term, even though your eye has healed fully, you should avoid engaging in activities that may result in trauma to the eye, such as martial arts and physical contact sports. At any rate, you must make sure you protect your eyes during the course of your normal daily activities.
How much vision you regain following surgery depends on:
– the extent of the retinal detachment
– involvement of the macula, which is essential for seeing fine detail)
– the presence of other eye diseases, such as diabetic retinopathy
– time taken before retinal detachment surgery was performed
Your peripheral vision should return after surgery, although there may be some restriction especially if the retinal detachment was extensive. If your macula was affected, you may notice some distortion and waviness in your central vision. Although this will not go away completely, most people are able to adapt to this over time.
As with all eye operations, there is a risk of developing complications after retinal detachment surgery. These include infection, cataract, glaucoma and persistent uveitis. In a small percentage of people, surgery is successful in re-attaching the retina but not in restoring vision. The risks of problems occurring and poor visual outcomes after surgery are higher the longer surgery is delayed.


