What is a pterygium?
A pterygium (plural: pterygia) is a benign growth of the conjunctiva (skin of the eye) that grows towards the cornea (front window of the eye). In some more aggressive cases, the pterygium grows onto the surface of the cornea. The somewhat unusual name comes from its triangular shape giving rise to a “wing-shaped” appearance. Remember: they are non-malignant and non-cancerous.
Pterygia tend to occur in those over the age of 20. They affect males twice as frequently as females. In the United States, occurrence ranges from 2% up to 15%, being more common nearer the equator. In parts of Australia, particularly the hotter and sunnier regions, prevalence has been estimated to be up to 10%.

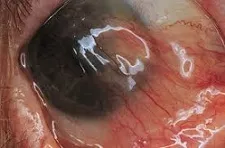
Examples of pterygia (white arrows). Left: mild with little advancement onto the cornea. Right: advanced with significant advancement onto the cornea, almost obscuring the visual axis.
What causes pterygia?
How pterygia develop is still not yet completely understood. There are probably multiple factors that contribute to the development of pterygia. One risk factor is injury or severe infection in the eye, which can lead to the start of a pterygium.
However, the single most important risk factor is ultraviolet light exposure. The longer and greater your exposure to the sun throughout your life, the higher your risk. This is why they are more common in tropical climates where people spend a lot of time outdoors. Susceptible groups include farmers, fishermen and gardeners. One of the ways of preventing pterygia from developing is by wearing 100% UV blocking sunglasses.
What problems can pterygia cause?
Most of the time, pterygia do not cause any problems apart from being something you are able to see on your eye. All you may notice is just a triangle-shaped piece of flesh over the corner of your eye.
However, if severe enough (example on the right), they can cause problems. The 3 main symptoms that you may experience from pterygia are poor cosmesis, irritation and reduction in vision.
Poor cosmesis: In some patients, the pterygium may look very fleshy and unsightly. In addition, it can also make the eye look constantly red and inflamed.
Irritation: Pterygia can also cause excessive irritation and discomfort in the eye. This can be due to dryness or a chronic foreign body sensation. Certain irritating circumstances, such as smoke-filled rooms, sunlight exposure, dust and wind exposure, fatigue and air-conditioning, can worsen the symptoms of discomfort.
Reduction in vision: It is uncommon for a pterygium to affect vision unless it is very advanced (see right). It may extend along the cornea far enough to obscure the pupil and prevent light from entering the eye. Sometimes, it can exert enough traction to deform the cornea, thus inducing irregular astigmatism.
How can pterygia be treated?
Most pterygia do not cause problems and can therefore be left alone. Some people prefer the reassurance of being monitored every so often by an ophthalmologist to check that there has been no progression. For those that require treatment, there are 2 main treatment options: eye drops and surgery.
Eye drops: Lubricating eye drops, such as those used in dry eye treatment, can help to soothe the eye and ease the discomfort. Occasionally, a short course of a non-steroidal anti-inflammatory eye drop (such as ketorolac or diclofenac) or a weak steroid drop (such as fluorometholone or rimexolone) may be required to settle excessive inflammation of the eye. Only artificial tears and topical lubricants are suitable for long-term use.
Pterygium surgery: Surgical excision and conjunctival autograft is indicated in the small proportion of patients in whom the pterygia are bad enough to affect the vision or to cause significant eye discomfort. Many surgical techniques and variations have been described, but the most commonly performed procedure is excision combined with a conjunctival autograft.
This procedure takes between 45 to 60 minutes and is done under local anesthetic as a day case procedure. After the pterygium is carefully excised, a part of your healthy conjunctiva is harvested to cover the exposed area. The conjunctival autograft is kept in place either with dissolvable stitches or with fibrin glue. Sometimes, a bandage contact lens is placed at the end of surgery.
Without a conjunctival autograft, a simple pterygium excision has a recurrence rate of up to 50%. Studies have shown that having a conjunctival autograft reduces the high recurrence rate down to around 5%. Transplanting healthy conjunctiva onto the affected area reduces the chance of the abnormal pterygium tissue growing again. Other methods of reducing recurrence during surgery include applying antimetabolites such as mitomycin-C and using radiotherapy. These are associated with potentially serious side effects and are therefore reserved for more difficult cases.
After surgery, you will need to use antibiotic eye drops (to reduce the risk of infection) and steroid eye drops (to reduce the inflammation in the eye) for about 6 weeks.
It normally takes around 6 weeks for the eye to settle, although there may still be some redness and occasional discomfort for a good few months. Please note that sometimes surgery can change your spectacles prescription sufficiently to require you to get a new pair of glasses.


