Why is glaucoma tube shunt implantation necessary?
Glaucoma tube shunt implantation is performed for patients with worsening glaucoma or uncontrolled high eye pressure despite being on medications.
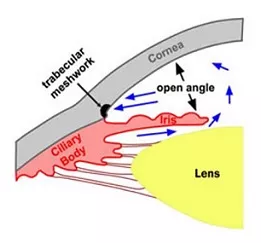
Fluid in the eye (aqueous) is produced by the ciliary body, and drains out through the trabecular meshwork (drainage pathway) in the drainage angle. Sometimes the trabecular meshwork no longer copes, preventing aqueous from draining out easily. This causes pressure to build up in the eyeball. When the pressure in the eye is too high, it can cause optic nerve damage and permanent vision loss – this is called glaucoma.
A functioning glaucoma tube shunt reduces the eye pressure, which in turn reduces the risk of further optic nerve damage from glaucoma.
The two glaucoma tube shunts currently available for use in Australia are the Baerveldt and Molteno tubes. Both are equally effective at reducing eye pressure. Other tube shunts include the Ahmed glaucoma valve implant and the Paul glaucoma implant.
See Related: Surgical treatments for glaucoma
What does the glaucoma tube shunt procedure involve?
Glaucoma tube shunt implantation is a 60 to 90 minute surgical procedure which involves:
● Applying an anti-scarring medication (mitomycin-C) to prevent scarring.
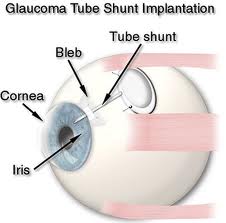
● Fixing the shunt plate to the wall of the eye, underneath the eye muscles.
● Occluding the tube to prevent uncontrolled aqueous drainage.
● Inserting the end of the tube into the eyeball.
● Placing donor sclera tissue over the tube insertion site to prevent erosion.
● Covering the operated area with the conjunctiva (transparent skin
overlying the sclera). This forms a pocket of fluid called a ‘bleb’.
Aqueous will drain from the eyeball via the tube into the bleb and become absorbed by surrounding blood vessels. This decreases the eye pressure.

What are the potential risks?
Glaucoma tube shunts have a success rate of around 70-80%. Most complications can be treated, although sight-threatening complications may occur rarely (less than 1 in every 1000). These can sometimes occur even if the operation has been carried out perfectly.
If you have severe glaucoma, there is a risk of completely losing all vision due to the stress of the procedure (snuff-out).>
Risks during surgery:
● Bleeding into the eye. If severe the operation may be discontinued, and
will need to be completed on another day.
● Damage to other parts of the eye. This will prolong the surgery and your
eye may take a few months to recover instead of a few weeks.
Risks after surgery, where treatment does not involve another procedure:
● Bruising of the eye or eyelids. This is quite common.
● Allergy to the post-surgery eye drops, causing redness and irritation of
the eye and eyelid.
Risks after surgery, where treatment requires another surgical procedure:
● High pressure in the eye. The pressure can be reduced by releasing
aqueous from the eye, or by taking pressure-lowering eye drops or
tablets. The intraluminal suture (stitch occluding the tube) is removed
after 3 months if the pressure remains persistently high.
● Low pressure in the eye (hypotony). This usually settles over the course
of several weeks to months. If prolonged and severe, the glaucoma tube
shunt may have to be removed.
● Tube shunt failure. Scarring of the shunt plate and bleb prevents aqueous
from draining out of the eye. During your postoperative visits, you may
receive multiple injections of anti-scarring medication (5-fluorouracil)
around the shunt plate and bleb to try to prevent the scar tissue from
forming. Sometimes the scar tissue needs to be cut with a blade or
needle to free up the shunt plate and bleb (bleb needling procedure).
● Infection inside the eye (endophthalmitis). This is the most serious
complication and may cause permanent sight loss despite treatment with
antibiotics and surgery.
● Cloudiness of the lens in the eye (cataract). This can be treated with
cataract surgery.
● Double vision. This may require surgery to adjust the muscles controlling
eye movements.
● Erosion of the tube shunt. This may require repositioning or removal of
the tube shunt.
● Droopiness of the eyelid (ptosis). This is usually mild. However if this
causes problems, the eyelid can be lifted by tightening the eyelid muscle
(ptosis surgery).
See Related: Risks and complications of glaucoma surgery
What should I expect?
Glaucoma tube shunt implantation is a hospital-based day case procedure usually performed under local anesthetic. The operation is usually performed one eye at a time.
Before surgery:
On the day of your procedure, please take all your usual medications unless otherwise advised. You will need to fast for at least 6 hours before your procedure. You will not be able to drive home on the day of the procedure, so you will need to arrange for someone to take you home. Please allow at least 3 to 4 hours in the hospital.
Before the procedure, you will receive the following:
● Cannula inserted into a vein, usually at the back of your hand.
● Local anaesthetic eye drops prior to the anesthetic injection.
● Local anesthetic injection into the eye socket to fully numb the eye.
During surgery:
To reduce the risk of infection, povidone iodine antiseptic is used to clean your eye and eyelashes, a sterile drape will cover your face, and a sterile clip will keep your eyelids open.
You will be awake during surgery, but you should not feel any pain. If you feel discomfort or pain, additional local anesthetic can be given. It is normal to notice bright lights or colors, hear buzzing and beeping sounds, and feel cold water running down your cheek or ear.
You will need to lie relatively still for up to 90 minutes for the operation. At the end of surgery, you may feel a sting due to an injection.
After surgery:
After the operation, a pad and shield will be placed over your eye. The pad and shield can be removed the next day, and you can start your postoperative eye drops. These comprise:
● Steroid anti-inflammatory eye drops (Prednisolone or Dexamethasone)
2-hourly for 4 to 6 weeks. These drops will be decreased gradually over
several months.
● Antibiotic eye drops (Chloramphenicol) 4 times daily for 1 week.
● Steroid eye ointment (Hydrocortisone) at night for 1 month.
You will need to stop your glaucoma eye drops (if any) to the operated eye. However, please continue your usual eye drops to the non-operated eye.
Over the next few weeks, you will experience blurriness, discomfort, sensitivity to light, and blood around the eye. These will gradually improve over several weeks with the eye drops.
You will be reviewed the next day, and then weekly for a few weeks after surgery. During these visits, you may receive injection of an anti-scarring medication (5-fluorouracil) around the bleb. The visits (and injections) will become less frequent as the eye settles.
Please contact the clinic immediately if you experience pain or a sharp drop in vision.
See Related: