
Why is it important to measure the corneal thickness?
Corneal thickness is one of the major considerations that determine if you can be eligible for flap-based laser refractive surgery (LASIK). You may have heard people saying that they are unable to undergo LASIK because their corneas are “too thin” or “not thick enough”. Before undergoing any form of laser refractive surgery, you should understand why corneal thickness measurements are essential.
LASIK works by removing (ablating) tissue from the cornea. This reshapes the surface of the cornea to correct the refractive error. The amount of corneal tissue that is removed from the stroma is call the ablation depth, and this depends on the degree of refractive error. In myopia, corneal tissue is removed from the center of your cornea to flatten the corneal surface. In hyperopia, corneal tissue is removed from the periphery of your cornea to steepen the corneal surface. The remaining underlying corneal tissue is called the residual stromal bed.
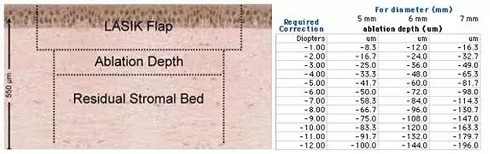
Left: There are 3 layers to consider when undergoing LASIK: the LASIK flap, the ablation depth, and the residual stromal bed. All 3 need to be factored in before LASIK can be performed. Right: The ablation depth depends on pupil diameter, degree of refractive error that needs to be corrected and LASIK system used.
In general, corneal thickness ranges from 500 to 600 micrometers. United States Food and Drug Administration (FDA) recommended that the residual stromal bed must be at least 250 micrometers thick. This 250 micrometer thickness of untouched corneal tissue is important because it preserves the integrity of the corneal tissue and reduces the risk of complications, in particular, corneal ectasia.

Corneal ectasia or keratectasia occurs when the corneal tissue is too thin to support the eyeball, resulting in the bulging out of the cornea and severe visual distortions. This can be initially treated with soft contact lenses but may eventually require special rigid gas permeable contact lenses, corneal implants and perhaps even a corneal transplant.
Due to this potentially devastating complication, most ophthalmologists prefer to leave up to 300 micrometers of residual stromal bed for extra safety and to allow for retreatments (enhancement) if required.
Besides laser refractive surgery, corneal thickness measurements are also important in the management of glaucoma. Thin corneas are associated with a higher risk of glaucoma.
Corneal thickness is usually measured with an ultrasound pachymeter. After your eye is numbed with anesthetic eye drops, the pachymeter probe will be placed in front of your eye, just touching the corneal surface. Measurements are automatically taken by the probe and then displayed on the monitor. There are other instruments that can measure corneal thickness without touching the eye. These include the Orbscan, Pentacam, and anterior segment OCT.
Example corneal thickness calculation – thick enough
In LASIK, there are different flap thicknesses and many algorithms and nomograms for ablation depth calculations. For the purpose of illustration, let’s use the typical LASIK flap thickness of 160 micrometers, and let’s say that for a 6 millimeter diameter pupil, every 1 diopter of prescription power requires the removal of 12 micrometers of corneal tissue.
Patient’s refractive error: -8.00 diopters
Amount to ablate: 8 x 12 = 96 micrometers
Thickness of patient’s cornea: 580 micrometers
LASIK flap thickness: 160 micrometers
Minimum residual stromal bed thickness: 250 micrometers
Available tissue for ablation: 580 – 160 – 250 = 170 micrometers
So in this example, the patient needs to ablate 96 micrometers from 170 micrometers of corneal stromal tissue. This means that the cornea is thick enough for LASIK to proceed. The residual stromal bed in this instance will be 324 micrometers, which is very safe and carries a lower risk of complications.
Example corneal thickness calculation – too thin
Patient’s refractive error: -14.00 diopters
Amount to ablate: 14 x 12 = 168 micrometers
Thickness of patient’s cornea: 510 micrometers
LASIK flap thickness: 160 micrometers
Minimum residual stromal bed thickness: 250 micrometers
Available tissue for ablation: 510 – 160 – 250 = 100 micrometers
So in this example, the patient needs to ablate 168 micrometers from 100 micrometers of remaining corneal stromal tissue. So the cornea is too thin to undergo LASIK. If LASIK were to be carried out, there will be an increased risk of corneal ectasia because of the thin residual stromal bed, which will only be 182 micrometers thick, well short of the 250 micrometers recommended by the US FDA.
What if your cornea is too thin?
If your cornea is too thin, it may still be possible for you to undergo laser refractive surgery. Your ophthalmologist may be able to create thinner flaps (less than 160 micrometers thick) with either the femtosecond laser or with special types of microkeratomes. Alternatively, you may wish to consider undergoing surface-based laser refractive surgery, where no corneal flaps are created. These techniques include PRK (photorefractive keratectomy), LASEK (laser assisted sub-epithelium keratomileusis) and Epi-LASIK (epithelial laser assisted in situ keratomileusis).



