Diabetic retinopathy is fast becoming a major public health problem worldwide. Diabetic retinopathy laser treatment and screening now consumes a significant amount of healthcare resources worldwide. Despite this, it remains the fifth commonest cause of blindness in the world. One million Americans have advanced diabetic retinopathy, which if untreated, may lead to permanent blindness. Every year, up to 25,000 adult Americans become blind from diabetic retinopathy.
Diabetic retinopathy is caused by diabetes mellitus. Blindness from diabetic retinopathy occurs due to diabetic maculopathy and proliferative diabetic retinopathy. However, these sight-threatening problems can be treated successfully with laser and with injections into the eyeball provided that treatment is given early enough. Remember that although diabetic retinopathy is the major cause of sight impairment from diabetes, there are also other diabetic-related eye diseases that can cause visual loss such as cataract, glaucoma, retinal vascular occlusion and ischemic optic neuropathy.
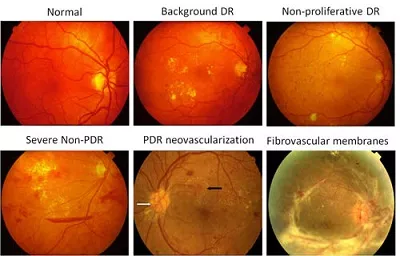
The various stages of severity of diabetic retinopathy, ranging from normal (top left) to end stage disease with severe scarring (bottom right).
Diabetic retinopathy laser treatment is the mainstay of treatment for sight-threatening diabetic retinopathy (but can be associated with side effects and complications). However, of equal importance is good control of diabetes and blood pressure to prevent advanced retinopathy from developing in the first place, and regular eye screening to detect signs of progression early. The earlier treatment is given, the better the outcomes. Other treatment options include intravitreal injections and vitrectomy surgery.
Diabetic macular edema laser treatment
Diabetic maculopathy is the most common cause of visual loss in diabetes. It occurs when your macula becomes affected by the retinopathy changes caused by diabetes. The 2 main types of maculopathy are diabetic macular edema (DME) and macular ischemia.
In diabetic macular edema, there is fluid leakage from the retinal blood vessels, causing the macula to thicken and swell up. Macular edema can be treated with laser and intravitreal injections. In macular ischemia, the tiny retinal capillaries to the macula close up and the macula does not receive enough blood supply for it to work properly. Unfortunately, there is currently no effective treatment for macular ischemia.
Focal / grid retinal laser: This is the main retinopathy laser treatment method for maculopathy from diabetic macular edema. The retinal laser seals retinal blood vessels that are leaking fluid and blood. This reduces further fluid and blood leakage, and reduces the swelling of the macula. The retinal laser may also somehow stimulate the retinal cells to ‘pump’ away any excess fluid at the macula. The laser is only directed at certain parts of the macula; the rest of the peripheral retina is untouched.
Focal retinal laser to the macula is usually performed in the consulting rooms without the need for a hospital visit. It involves first dilating your eyes and then numbing your eyes with drops. After that, a contact lens is placed on your eye to allow a clear view of the area to laser. You will see a red aiming beam during laser – this aiming beam allows your ophthalmologist to target the area to be lasered. Do NOT look directly at this light. If you do, the very center of your macula could be directly lasered and this may cause permanent loss of your visual acuity and central vision. Your vision should not be affected by the laser otherwise. Focal retinal laser treatment is quick and may sometimes only take a few minutes.
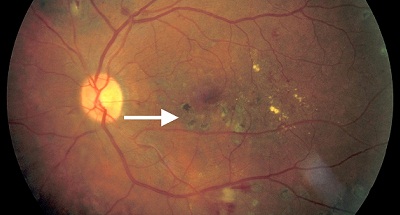
Focal laser treatment for diabetic macular edema leaves behind laser scars which are seen as black marks on the macula (white arrow).
Not everyone with diabetic macular edema requires retinopathy laser treatment. Laser is only required for those with vision worse than 20/40 and clinically significant macular edema, which is defined as swelling of the retina occurring within 500 micrometers of the center of the macula by the Early Treatment Diabetic Retinopathy Study (ETDRS). An important point to remember is that the aim of retinal laser treatment is not to improve your vision but to prevent it from getting worse.
Focal retinal laser treatment is now often combined with intravitreal injection of either steroid or anti-Vascular Endothelial Growth Factor (anti-VEGF) into the eyeball to improve visual outcomes. Steroid such as triamcinolone and anti-VEGF drugs such as bevacizumab and ranibizumab work by interfering with chemicals that encourage leakiness of the retinal blood vessels at the macula. This helps to reduce the swelling of the macula and prevents further damage to your sight. It is thought that by combining treatments, there will be an additive effect resulting in better visual outcomes.
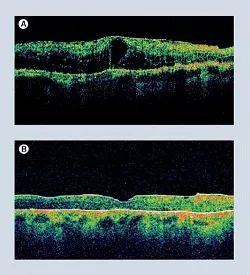
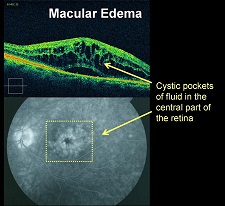
The picture on the left shows successful treatment for diabetic macular edema.
Top (A): Macular swelling and thickening before treatment. Leakage from the retinal blood vessels causes fluid to accumulate in the macula. This disrupts the function of the macula and causes reduced vision.
Bottom (B): The fluid in the macula has now cleared. Notice how the macula has returned to its original thickness and architecture.
Proliferative diabetic retinopathy laser treatment
Proliferative diabetic retinopathy (PDR) is the most advanced form of diabetic retinopathy. Proliferative diabetic retinopathy is characterized by the growth of abnormal new blood vessels (neovascularization) in the eye. Neovascularization occurs as a natural response to the retinal cells being starved of oxygen and nutrient due to the blockage of the retinal blood vessels from diabetes.
These abnormal new blood vessels grow in the wrong place on the surface of the retina and into the vitreous gel. They cause visual impairment when they bleed into the vitreous cavity of the eye (vitreous hemorrhage) or when they cause scar tissue formation which then pulls on and detaches the retina (tractional retinal detachment).

Pan-retinal photocoagulation (PRP): The first line of proliferative diabetic retinopathy laser treatment is with panretinal laser photocoagulation or scatter photocoagulation. As the name suggests, this treatment involves lasering large areas of the retina with the aim of coagulating or burning the ischemic retinal cells in the retinal periphery.

After panretinal laser, the ischemic cells throughout the retinal periphery become replaced by scar tissue. This reduces the production of chemicals that stimulate the growth of the abnormal new blood vessels.
If proliferative diabetic retinopathy laser treatment is performed at the early stages, the abnormal new blood vessels may regress and eventually disappear completely. This would eliminate the risk of vitreous hemorrhage and tractional retinal detachment from diabetic retinopathy altogether. If proliferative diabetic retinopathy laser treatment is performed only at the later stages, further abnormal new blood vessels will be prevented from forming. However, existing abnormal vessels may not regress completely. In this situation, the risk of vitreous hemorrhage and tractional retinal detachment is reduced but not eliminated.
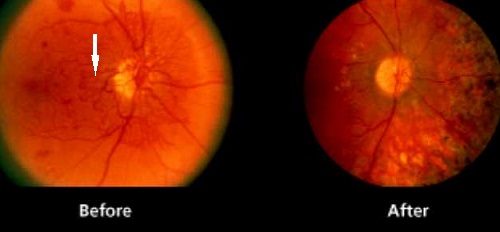
Abnormal new blood vessels can be seen on the optic disc before panretinal laser photocoagulation (white arrow; left). The new blood vessels completely regressed following successful laser treatment (right). Note the retinal laser scars on the right of the optic disc.
As with focal laser treatment, panretinal laser is also performed in the consulting rooms without the need for a hospital stay. After dilating and numbing your eyes with drops, a contact lens is placed on your eye to stop your eye from blinking and to allow visualization of the parts of the retina to be lasered.
Due to the extensive nature of the laser, it can be quite uncomfortable during laser. There are ways to reduce the discomfort from laser. Taking some pain-relieving or anti-inflammatory medications before laser will lessen any discomfort. The panretinal laser treatment can be also split into 2 or 3 treatment sessions to reduce the intensity of each session. If still intolerable, a subtenon injection of anesthetic can be given around the eye to completely numb the eye. Tell your ophthalmologist if laser is uncomfortable so that something is done about it – nothing is worse than having to suffer in silence.
Panretinal laser photocoagulation is also often combined with injections of anti-VEGF into the eyeball to improve visual outcomes. The anti-VEGF drugs interfere with chemicals that encourage the growth of abnormal new blood vessels, and so will act in concert with the conventional diabetic retinopathy laser treatment to improve visual outcomes.


