
I heard that cataract surgery is really safe now. Does this mean that cataract surgery no longer has complications?
The advances in technology and surgical techniques has resulted in the high success rates of cataract surgery worldwide. So many people now have had successful cataract operations, and some are now talking about cataract surgery as being only a ‘minor’ procedure.
Does this mean that cataract surgery complications are a thing of the past?
Unfortunately no, complications can still occur from cataract surgery, even in the most experienced of surgical hands.
It is common to have some discomfort, grittiness, sensation of something in the eye, and blood on the surface of the eye after surgery.
The great majority of problems are mild and will clear up over a few days to a few weeks without treatment, or are easily treated without long term consequences.
More serious complications are uncommon and occur in only around 3% of cases. Occasionally, a second operation will be needed to fix problems from the cataract operation.
Severe cataract surgery complications resulting in blindness are very rare (less than 0.1%).
See Related: Patient information guide to cataract surgery
When do cataract surgery complications occur?
Cataract surgery complications can occur during surgery itself, within a few days or weeks of surgery (early complications), and months after surgery (late complications).
Often, these complications occur not because of anything you have or have not done.
If at any point after your surgery, you are concerned that you may have developed any complications, please consult your ophthalmologist without delay. It is better to be safe and get your eye examined. The last thing you should worry about is ‘wasting’ your ophthalmologist’s time.
See Related:
Complications occurring early after cataract surgery
Complications occurring late after during cataract surgery
Can you tell me more about the possible late cataract surgery complications?
All forms of eye surgery are at risk of late complications that occur months after the initial surgery, and cataract surgery is no exception.
In this section, I discuss three of the more common and significant late cataract surgery complications: posterior capsular opacification, intraocular lens dislocation, and retinal detachment. These complications can occur even though the initial surgery was highly successful.
1. Posterior capsular opacification (PCO)
The capsule is the thin membrane that forms a bag that supports the lens inside your eye. During surgery, the cataract is removed from the capsule, and a synthetic intraocular lens implant is inserted into the capsule in place of the cataract.
Posterior capsular opacification occurs when this thin membrane becomes cloudy from growth of scar tissue. The scar tissue blocks and reduces the amount of light that can pass through the lens implant, causing blurriness of the vision.
PCO is quite common, occurring in approximately 20% of cases after cataract surgery.
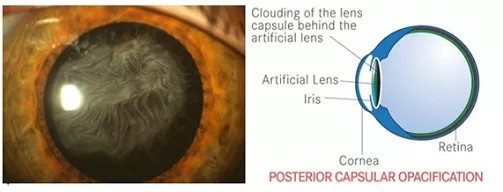
Symptoms of PCO: Often, you find that your vision gradually becomes misty again, almost like what it was before your cataract operation.
Treatment for PCO: Posterior capsular opacification does not go away by itself. However, it is easily treated with laser capsulotomy and takes no more than 5 minutes. Laser capsulotomy effectively ‘punches’ a hole through the cloudy capsule; this allows light to pass freely into your eye and thus enables you to see clearly again. This laser procedure is quick, safe. effective, and can be done in the consulting rooms.
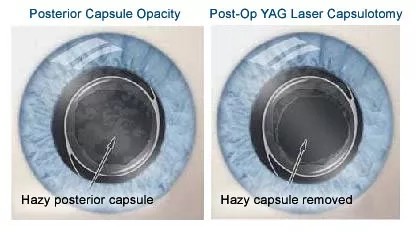
Posterior capsular opacification is easily treated with YAG laser posterior capsulotomy. The laser creates a central opening in the middle of the cloudy membrane.
2. Intraocular lens dislocation
Usually, the intraocular lens remains implanted in its capsular bag in the eye permanently. There is no requirement to remove or to replace the intraocular lens unless specifically indicated.
However in certain situations, the capsular bag stability may weaken, resulting in intraocular lens subluxation (the lens has moved partially) or dislocation (entire intraocular lens has dislodged from its original implanted position).
This may happen in eyes with difficult surgery, from trauma, and also pre-existing weakness of the zonules from conditions such as pseudoexfoliation.
Symptoms of lens dislocation: When the lens implant has moved, it is no longer focusing light onto the retina. Your vision will become blurry and feel unfocused.
Treatment of lens dislocation: Treatment depends on how much the intraocular lens has moved, how much vision is affected and whether there is damage to other ocular tissues. If there is mild subluxation and you are still able to see reasonably clearly, then there is no need to intervene. If the entire intraocular lens is dislocated into the vitreous cavity, you will generally need vitrectomy surgery to remove the dislocated lens followed by secondary lens implantation.
3. Retinal detachment
The retina is the innermost layer of the eye, and it functions to convert light into biochemical signals which are then transmitted to the brain. Retinal detachment occurs when the retina peels away from the wall of the eye.
This occurs in 0.5% of patients after cataract surgery. It is more common in cataract operations that have experienced complications during surgery. Retinal detachment will cause blindness if the retina is not put back in place in a timely manner.
Symptoms of retinal detachment: There are 3 main symptoms to look for: flashing lights, floaters, and a shadow or curtain obscuring your field of vision. If you notice any of these, please consult your ophthalmologist without delay.
Treatment for retinal detachment: Retinal detachments can only be treated with retinal detachment surgery. In the case of retinal detachment following cataract surgery, the surgery will most likely be a vitrectomy procedure combined with laser and oil or gas injection.
See Related: Patient guide to vitrectomy for retinal detachment
Final word about complications after cataract surgery
I think this is worth reiterating: If you had cataract surgery recently, and you are concerned that you may have developed any complications, please consult your ophthalmologist without delay. It is better to be safe and get your eye examined.
Most of the time, it will turn out to be nothing. But if something has indeed occurred, then it is better to be treated early for the best possible outcome.
If you are interested to learn more about the specifics of cataract surgery complications, below are a selection of books and other items that you may find helpful.


