Glaucoma surgery is effective in lowering eye pressure, but can be associated with surgical complications, some sight-threatening, but mostly minor. Most of the time, you will have a good outcome if they are dealt with promptly and managed properly. Some complications are more difficult to manage than others, and may require repeat surgery and/or frequent outpatient visits.
Early glaucoma surgery complications
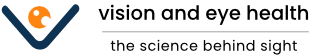
Hypotony: Hypotony is when the pressure in the eyeball becomes too low (below 6 mmHg). This means that the operation has been too successful in draining out the aqueous fluid and lowering the eye pressure. Unfortunately, having eye pressure that is too low is not good for the eye. Low eye pressure affects the function of the macula and causes visual loss (hypotony maculopathy). Hypotony is the commonest cause of blurry vision after glaucoma surgery. Mild hypotony tends to settle by itself. However, if the hypotony is more severe and persistent, another operation will be required to fix it.
Left (A): Low eye pressure causing optic disc swelling and hypotony maculopathy. Right (B): The optic disc and macula return to their original state once the hypotony is fixed.
Infection of the eyeball (endophthalmitis): Endophthalmitis is one of the most dreaded complications of any ocular surgery surgery. It is extremely serious, and you can lose your vision permanently. How would you know if you have endophthalmitis? Well, your eye will be extremely painful and you will have very poor sight. There may be yellow discharge from the eye and you may even see a yellow fluid level in the eyeball (hypopyon). This condition is an ophthalmic emergency, so please do not wait and see “if it gets better over the next few days”. It won’t. Your eye needs immediate injection of antibiotics into the eyeball. You will most likely be admitted to hospital for intensive eyedrops and oral medications. The earlier treatments are started, the better the chances of retaining good vision. However, it can take several months before the eye settles down.

Postoperative infective endophthalmitis is one of the worst possible complications to occur following glaucoma surgery. This is infection affecting the entire eye, and if not treated expediently with antibiotic injections into the vitreous cavity, will result in permanent blindness. Note the yellow fluid level or hypopyon in this eye.
Luckily, this condition is very rare (less in 0.1%) due to the meticulous cleaning and infection control techniques. If you have a condition that lowers your immune system and predisposes towards infection, highlight it to your ophthalmologist so that even more precautions can be taken to prevent infection.
Late glaucoma surgery complications
Scarring: In up to 20% of cases, severe scarring occurs and closes the drainage channel from glaucoma surgery. This causes the eye pressure to increase again. Scarring is the major cause of failure of pressure lowering operations. Scarring is more severe in young people, people of African descent, those with inflammatory disease and those who have had previous eye surgery. Sometimes a procedure called bleb needling can open up the scarred area and restore drainage. In bleb needling, the tip of a fine hypodermic needle is used to cut the scarred area that is closing off the drainage channel. Anti-scarring medication is usually also injected at the time of bleb needling to try to keep the drainage channel working.

Scarred trabeculectomy bleb with injected blood vessels around it. Multiple bleb needlings and injections of anti-scarring medications may be required to re-establish aqueous drainage.
Cataract: This is one of the more common glaucoma surgery complications. A cataract develops when the natural lens becomes cloudy, and this occurs naturally as you grow older. Having glaucoma surgery disrupts the environment of the eye and quickens this process. If the cataract causes your vision to become blurry, then you will require cataract surgery. Sometimes, undergoing cataract surgery can sometimes cause the drainage channel from glaucoma surgery to scar up and fail. To prevent this from happening, an injection of anti-scarring medication is usually given at the time of cataract surgery.
Blebitis: Glaucoma surgery often results in the formation of a ‘bleb’, which is an area of conjunctival elevation due to accumulation of fluid that is draining out from the eye. In blebitis, the bleb (particularly thin-walled and leaking ones) becomes infected.

Your eye will become red and painful, and you may see a collection of pus in the bleb area, such as in the example above. Blebitis is one of the more serious glaucoma surgery complications and must be treated promptly to prevent the infection from spreading to the back of the eye. Treatment is with intensive antibiotic and steroid eye drops.
Drainage implant complications: These are specific for drainage implants, where a silicone tube is inserted into the eyeball at one end and secured to a plate at the other end. The tube in the eyeball has to sit in the anterior chamber between the cornea and the iris, without touching either. If the tube touches the cornea, this can result in corneal decompensation, where the cornea becomes cloudy. If the tube rubs against the iris, this can cause uveitis (inflammation of the eye). The tube can also erode out of the eyeball. These glaucoma surgery complications tend to occur late and will need to be fixed surgically.

An example of tube erosion following drainage implant surgery. The red circle shows the location of the protruding tube. The tube will need to be reimplanted into the eye or be removed. Your eye will be at risk of developing infection if this is not corrected.