
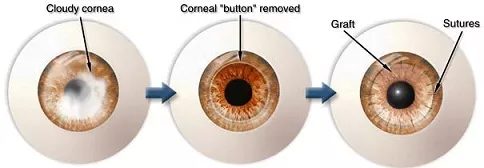
What is corneal transplant surgery?
In corneal transplant surgery, unhealthy, cloudy cornea (front window of the eye) is replaced with healthy, clear cornea from a donor. Most of the time, you will have a good outcome with improved vision after surgery. However, to maintain the success of the operation, potential corneal transplant complications need to be monitored for regularly and treated in timely manner. Some complications are more difficult to manage than others, and may require repeat surgery and/or frequent outpatient visits.
It is important that you listen and adhere to the advice given to you by your ophthalmologist regarding your eye drops and general care after surgery. Doing so reduces the risk of corneal transplant complications and increases the chance of success of your operation.
Corneal transplant complications can be classified into early (within 2 weeks of surgery) and late (after 2 weeks postoperatively) complications.
Early corneal transplant complications
Wound and suture complications: Occasionally, there is leak of aqueous from inside the anterior chamber of the eye through the edge of the corneal graft. This may be due to loose, broken or insufficient sutures. Prolonged leaking after a corneal transplant operation can result in infection and hypotony (low pressure in the eyeball), with both potentially causing visual loss. This is usually easily treated with a bandage contact lens or with extra stitches to the corneal graft.
Increased pressure in the eye (raised intraocular pressure): This can be uncomfortable, and happens in around 10% of the time. If the pressure increase is high, you may experience blurring and aching around the eye, as well as nausea and sickness. The raised pressure is usually temporary. Depending on how high the eye pressure is, your ophthalmologist may give you eye drops or tablets to bring the pressure down. This usually does not cause any lasting damage unless you already suffer from glaucoma.

Measurement of the intraocular pressure is important during the immediate postoperative period after corneal transplant surgery. Sometimes, the eye pressure may be high enough to require treatment. This is particularly important for those who have pre-existing glaucoma.
Infection of the eyeball (endophthalmitis): Endophthalmitis is one of the most dreaded complications of any ocular surgery surgery. It is extremely serious, and you can lose your vision permanently. How would you know if you have endophthalmitis? Well, your eye will be extremely painful and you will have very poor sight. There may be yellow discharge from the eye and you may even see a yellow fluid level in the eyeball (hypopyon). This condition is an ophthalmic EMERGENCY, so please do not wait and see “if it gets better over the next few days”. It won’t. Your eye needs immediate injection of antibiotics into the eyeball. You will most likely be admitted to hospital for intensive eyedrops and oral medications. The earlier treatment is started, the better the chances of retaining good vision. However, it can take several months before the eye settles down.

Postoperative infective endophthalmitis is one of the worst possible complications to occur following corneal transplant surgery. This is infection affecting the entire eye, and if not treated expediently with antibiotic injections into the vitreous cavity, will result in permanent blindness. Note the yellow fluid level or hypopyon in this eye.
Luckily, this condition is very rare (less in 0.1%) due to the meticulous cleaning and infection control techniques. If you have a condition that lowers your immune system and predisposes towards infection, highlight it to your ophthalmologist so that even more precautions can be taken to prevent infection.
Late corneal transplant complications
Corneal graft rejection: Rejection develops when your body recognizes the graft as foreign and tries to attack it. This occurs in around 10% to 20% of patients. Rejection is most common in the first year after surgery, but can happen at any time, even after many years of not having any problems. If detected early, it can be treated and the process reversed successfully. Treatment is usually with steroid eye drops, although sometimes steroid injections or tablets may be required.
You will need lifetime follow-up for your corneal graft because of the risk of rejection. You are at higher risk of rejection if you have:
– Blood vessels growing into the cornea from previous infection
– Previous corneal transplant surgery
– Other concurrent eye disease
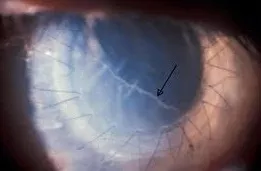
An example of corneal graft rejection. One of the characteristic signs of graft rejection is the Khodadoust line (black arrow), which is the accumulation of inflammatory cells at the corneal endothelium. Symptoms include redness of the eye, reduced vision and light sensitivity. If you notice any of these symptoms, consult your ophthalmologist immediately.
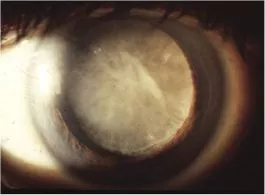
Corneal graft failure: This occurs when the graft no longer works. The cornea becomes cloudy and opaque again, thereby affecting your vision. Corneal graft rejection is an important cause of graft failure. Other important causes of corneal graft failure include recurrence of the original disease (such as keratoconus and herpes infection of the cornea), glaucoma and endothelial cell failure causing the cornea to become swollen with fluid.
Cataract: A cataract (see right) develops when the natural lens becomes cloudy, and this occurs naturally with age. Corneal transplant surgery and long-term use of steroid eye drops both quicken the process of cataract formation. If the cataract causes your vision to become blurry, then you will require cataract surgery.
Astigmatism: This is one of the most common corneal transplant complications. Astigmatism is due to the shape of the eye being irregular, such that it is shaped more like an oblong football rather than a basketball. Some degree of astigmatism is expected after surgery. Usually, astigmatism can be corrected with spectacles or contact lenses. If you have high amounts of corneal astigmatism, some of the sutures may be removed in stages to reduce it. It can take up to two years (when most, if not all, the sutures will have been removed) for your vision to stop fluctuating and achieve its best visual outcome. Laser vision correction may be appropriate in some cases to further improve vision.


