I heard that cataract surgery is really safe now. Does this mean that cataract surgery no longer has complications?
The advances in technology and surgical techniques has resulted in the high success rates of cataract surgery worldwide. So many people now have had successful cataract operations, and some are now talking about cataract surgery as being only a ‘minor’ procedure.
Does this mean that cataract surgery complications are a thing of the past?
Unfortunately no, complications still can occur from cataract surgery, even in the most experienced of surgical hands.
It is common to have some discomfort, grittiness, sensation of something in the eye, and blood on the surface of the eye after surgery.
The great majority of problems are mild and will clear up over a few days to a few weeks without treatment, or are easily treated without long term consequences.
More serious complications are uncommon and occur in only around 3% of cases. Occasionally, a second operation will be needed to fix problems from the cataract operation.
Severe cataract surgery complications resulting in blindness are very rare (less than 0.1%).
See Related: Patient information guide to cataract surgery
When do cataract surgery complications occur?
Cataract surgery complications can occur during surgery itself, within a few days or weeks of surgery (early complications), and months after surgery (late complications).
Often, these complications occur not because of anything you have or have not done.
If at any point after your surgery, you are concerned that you may have developed any complications, please consult your ophthalmologist without delay. It is better to be safe and get your eye examined. The last thing you should worry about is ‘wasting’ your ophthalmologist’s time.
See Related:
Complications occurring late after cataract surgery
Complications occurring during cataract surgery
Can you tell me more about the possible early cataract surgery complications?
All forms of eye surgery are at risk of early complications that occur within days after the initial surgery, and cataract surgery is no exception.
In this section, I discuss five early cataract surgery complications: hematoma around the eye, corneal edema, raised eye pressure, cystoid macular edema, and endophthalmitis. These complications can occur even though the initial surgery was highly successful.
1. Hematoma (bruising) around the eye
Your eye and eyelid may look and feel bruised. This is relatively common and will settle over a week or two. You may also notice some double vision, which will also clear up within a week without treatment.

Eye bruising after cataract surgery may look unsightly, but will resolve over a few days without affecting the recovery of the eye. It is more common in those who had peribulbar or retrobulbar anesthesia for surgery.
2. Corneal edema (swelling of the cornea)
The cornea is the clear window at the front of your eye, and its function is to allow light to enter into the eyeball. There is no fluid within a normal cornea. Sometimes after cataract surgery (around 1 in 10 operations), fluid accumulates in the cornea and causes it to become swollen.
Symptoms of corneal edema: The swelling in the cornea causes the sight to become cloudy, and may cause some pain.
Treatment of corneal edema: Corneal edema after cataract surgery is usually temporary and will go away without treatment after a few days. No extra treatment is generally needed beyond the usual anti-inflammatory eye drops after surgery. Sometimes, hypertonic (concentrated) saline is prescribed to hasten the recovery process
It is very rare (less than 1%) for the cloudiness in the cornea to become permanent. This is more likely to be an issue if you have a pre-existing corneal disorder, such as Fuch’s endothelial dystrophy or previous infection of the cornea. If this happens, you may need a corneal transplant operation to see better again.
Corneal edema is the accumulation of fluid in the corneal stroma. This reduces the amount of light that can pass through the cornea, causing the hazy appearance. Mild corneal edema is expected after surgery; this is generally transient and will settle after a week or so. No extra treatment is needed beyond the usual anti-inflammatory eye drops after surgery. Rarely, the edema remains persistent and requires treatment with a corneal transplant.

3. Ocular hypertension (increased eye pressure)
Around10% of the time, the eye pressure is high after cataract surgery. This usually occurs within the first 2 days of surgery.
Elevated pressure after surgery can be caused by inflammation in the eye, retained viscoelastic in the anterior chamber, and sometimes even from the steroid anti-inflammatory eye drops.
The pressure elevation usually does not cause any lasting damage unless you already suffer from glaucoma.
Symptoms of high eye pressure: This depends on how high the pressure is. Symptoms range from mild blurring to significant aching around the eye associated with vision loss and nausea. The latter indicates that the eye pressure is extremely high (over 40 mmHg), and requires urgent treatment.
Treatment of high eye pressure: The increased eye pressure is usually temporary, but often requires some form of short-term treatment. This is usually in the form of eye drops that you have to use for a few weeks.
If the eye pressure is very high in the first couple of days after surgery, your ophthalmologist may physically release some fluid from the eye, or give you a course of acetazolamide tablets to reduce the pressure.
In rare circumstances, the eye pressure cannot be controlled despite the measures above. If this happens, you will need a glaucoma operation to decease the pressure.
See Related:
Patient guide to trabeculectomy surgery for glaucoma
Patient guide to XEN stent implantation for glaucoma

Measurement of the intraocular pressure is important during the immediate postoperative period after cataract surgery. Sometimes, the eye pressure may be high enough to require treatment. This is particularly important for those who have pre-existing glaucoma.
4. Cystoid macular edema (swelling of the macula)
The macula is the central part of the retina and is vital for activities requiring central vision, such as when you are reading a book, watching television or looking at road traffic signs. Fluid may build up in the macula between 2 and 12 weeks after cataract surgery. When it happens, you’ll notice that your vision becomes blurry after a period of clear vision. This usually settles after a few weeks without treatment and problems. More often, you will be given a course of anti-inflammatory eyedrops to encourage recovery. In some cases, there will still be some residual visual blurring, despite complete resolution of the cystoid macular edema. This is more common after complicated cataract surgery and if the lens capsule had been ruptured. If you have age-related macular degeneration or diabetic retinopathy, then you are prone to this even if surgery was routine.
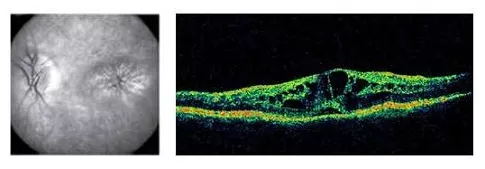
Cystoid macular edema (CME) occurs when fluid accumulates within the retinal architecture at the macula. This disrupts the macular function and thus causes reduced vision.
5. Endophthalmitis (infection in the eyeball cavity)
Of all the possible cataract surgery complications, endophthalmitis is one of the most dreaded. Endophthalmitis occurs when bacteria (or fungal microorganisms) infiltrate into the eyeball and spread infection throughout the eye. It is extremely serious, and you can lose your vision permanently if not treated urgently.
Symptoms of endophthalmitis: Your eye will be extremely painful and you will have little to no vision. There may be yellow discharge from the eye and you may even see a yellow fluid level in the eyeball (hypopyon). This condition is an ophthalmic emergency, so please do not wait to see ‘if it gets better over the next few days’. It won’t.
Treatment of endophthalmitis: Your eye needs an immediate injection of antibiotics into the eyeball. You will most likely be admitted to hospital for intensive eyedrops and oral medications. Vitrectomy surgery may be required to clear out all the infection in the eyeball cavity, particularly if the visual acuity is poor (hand movements or worse).
The earlier treatment is started, the better the chances of retaining vision. If you develop endophthalmities, it will take several months before the eye settles down.
See Related: Patient guide to vitrectomy surgery

Postoperative infective endophthalmitis is one of the worst possible complications to occur following cataract surgery. This is infection affecting the entire eye, and if not treated expediently with antibiotic injections into the vitreous cavity, will result in permanent blindness. Note the yellow fluid level or hypopyon in this eye.
Endophthalmitis is very rare (less in 0.1%) due to the meticulous cleaning and infection control techniques. If you have a condition that decreases your immune system and increases your infection risk, please highlight it to your ophthalmologist so that additional precautions can be planned for.
See Related: How to reduce your risk of endophthalmitis
Final word about complications after cataract surgery
I think this is worth reiterating:
If you had cataract surgery recently, and you are concerned that you may have developed any complications, please consult your ophthalmologist without delay. It is better to be safe and get your eye examined.
Most of the time, it will turn out to be nothing. But if something has indeed occurred, then it is better to be treated early for the best possible outcomes.
If you are interested to learn more about the specifics of cataract surgery complications, below are a selection of books and other items that you may find helpful.


